
Residency is a critical period to address representation
For learners from underrepresented groups — especially Black learners — the grueling years of effort to matriculate and earn an undergraduate degree, to be accepted into medical school, and to complete rigorous academic and clinical training to become an MD, DO, or PA can be derailed in the home stretch of graduate medical education, or residency.
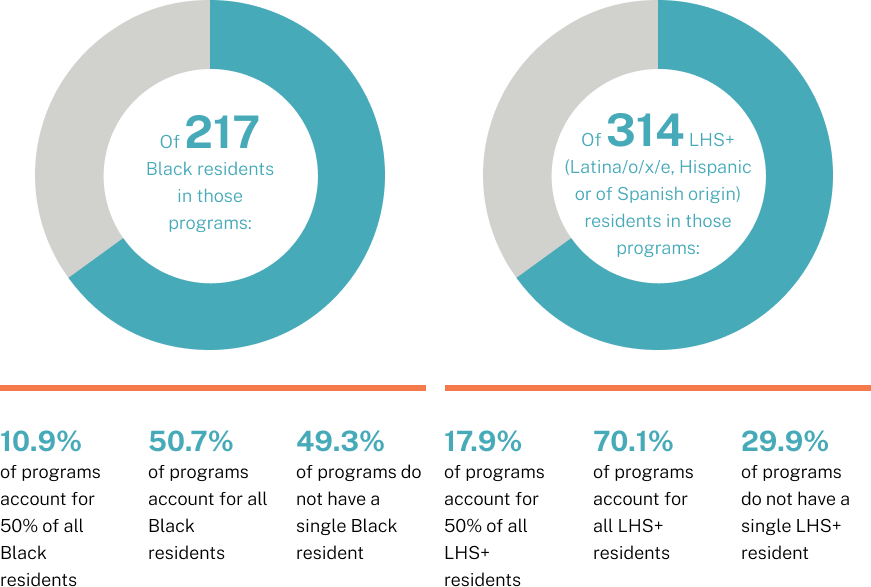
While growing attention has been focused on enrollment data, reasons for erosion of representation in this critical phase of training have been more elusive to assess. One thing that’s clear, as reported in 2022 by STAT, is that Black residents either leave or are terminated from residency programs at far higher rates than white residents. While Black residents account for about 5% of all residents, they accounted for nearly 20% of those who were dismissed in 2015, according to an unpublished analysis by the ACGME.
Data on this phenomenon continues to emerge and seems to apply particularly to specialties that have been historically dominated by white residents such as neurosurgery, dermatology, or plastic surgery. Which suggests why these fields have been unable to significantly diversify their ranks, even as the total number of residency spots has increased nationally. At Emory University, for example, there were five Black neurosurgeons among the 160 who graduated from residency programs in 2010, but four who left. In 2019, nine Black neurosurgeons finished residency, while three left. In this final stage of training, young physicians are vulnerable to subjective evaluations with potential for bias. Many report being advised by faculty out of surgical specialties toward family medicine or pediatrics, without regard for the type of medicine they'd like to practice.
And that’s the graduates who get matched into a program at all. There are more graduate medical students than there are residency slots, leaving Black students disproportionally unmatched in the year following graduation. Which is why expanding opportunities and prioritizing support to increase diversity in residency programs is one of the strategic priorities of the More in Common Alliance. By tripling the number of residency slots nationwide, we’ll address the issue in partnership with hospitals that welcome diverse learners to their programs and are committed to providing the supportive environment needed to increase the diversity of their medical providers.
In 201 total five-year Orthopedics core programs
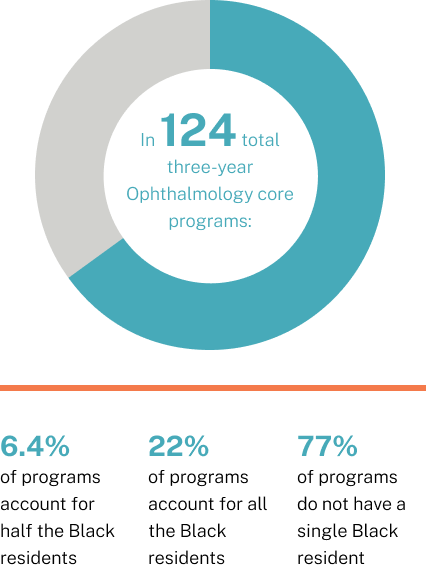
In 124 total three-year Ophthalmology core programs
A structured, strategic process
Over its ten-year focus, the More in Common Alliance has set the ambitious goal of expanding residency training capacity threefold, to nearly 400 slots sited at ten CommonSpirit Health facilities in strategic locations across the country. This expansion will not only afford a greater proportion of underrepresented graduates the opportunity to complete their training with less delay, it will also increase the likelihood that those trained physicians will put down roots in these communities, improving representation and access in the places that need it most.
Research shows that the majority of new physicians remain to practice in the community where they completed their residency. Which is why, to complement its undergraduate medical education initiatives, the graduate medical education effort will be strategically aimed to address physician shortages and other barriers to care in underserved and rural communities. Where a residency program is established, future care — and more culturally competent care — will logically follow.

Plan: site, specialty, and staffing considerations
Establishing a residency program requires a significant investment of resources, starting with identifying hospital sites. Even where there is mutual interest and an identified need, meeting the extensive requirements for patient volume, ambulatory care, and specialty exposure dictated by the Accreditation Council for Graduate Medical Education (ACGME) takes thorough consideration.
Progress: underway with expansion
The first More in Common Alliance residency program at Dominican Hospital in Santa Cruz, California onboarded its first class of residents in Summer 2024. Three additional California sites are in varied assessment stages in Bakersfield, Oxnard, and Los Angeles. A hospital in Chattanooga, Tennessee is under review as a potential site with a rural medicine focus.

People and Progress: perspective from the field
Casey Kirkhart, DO
Core Faculty, Family Medicine
Chief Medical Officer and Site Director, Santa Cruz Community Health FQHC
"The residents will have exposure to our entire practice — they’ll be part of our team. They’ll have their own panel of patients assigned to them, and they’ll be the primary care providers for those patients.”

Find out more about
- Enrollment at Morehouse School of Medicine
- Regional training sites at CommonSpirit Health facilities
- Community outreach to middle school, high school, and undergraduate learners
- Health equity and representation
- Staying informed about these issues
- Making a gift to support the More in Common Alliance